Abstract
Background - According to recommendations, AML patients with intermediate- or adverse-risk genetics are candidates for allogeneic SCT in first complete remission (CR1). In practice, only a minority of them undergoes SCT because of older age, comorbidities, poor tolerance of prior therapy, inability to achieve CR, or early relapse. The benefit associated with RIC-SCT is particularly difficult to assess in older patients, due to lower SCT numbers and strong selection biases.
Patients & Methods - Between 2012 and 2016, 509 patients aged ≥60 years (median, 68 years [60-85]) were enrolled in the prospective older AML ALFA-1200 trial. Eighty-eight patients (17%) had secondary or therapy-related AML. ECOG performance status was 0/1/2/3/NA in 219/219/57/9/5 patients and comorbidity index (HCT-CI) was 0/1/2/3/4+/NA in 226/92/66/61/54/10 patients, respectively. Risk subgroup distribution was 76 favorable (15%), 347 intermediate (68%), and 86 adverse (17%), according to the ELN-2010 classification retaining double mutations only as favorable CEBPA mutations. Chemotherapy consisted of cytarabine (200 mg/m2/d CIV on day 1-7) and idarubicin (12 mg/m2/d on day 1-3) followed by 2 courses with intermediate-dose cytarabine at 1500 mg/m2/12h on days 1/3/5, reduced to 1000 mg/m2/dose in patients aged ≥70 years. Patients with intermediate- or adverse-risk AML and/or those who needed two courses to reach CR were eligible for allogeneic SCT in CR1 if a suitable donor (HLA-identical [id] sibling or 9-10/10 matched unrelated donor) and no acquired contra-indication.
Overall Results - During first induction, 43 patients died before response evaluation, while 335 patients reached CR. Among the 131 patients with resistant AML, 71 received a second intensive course and 34 achieved CR (overall CR rate, 72.5%). The 60- and 100-day mortality rates were 9.4 and 13.0%, respectively. With a median follow-up of 26 months, 201/369 CR patients relapsed and 164 died, including 30 deaths in CR1. Median overall survival (OS) was 20.7 months (95% CI, 17.5-24.8) and OS was 46.8% (95% CI, 41.9-51.4) at 2 years. Median OS was 49.7, 22.5 and 9.4 months in the favorable, intermediate and adverse ELN-risk subgroup, respectively.
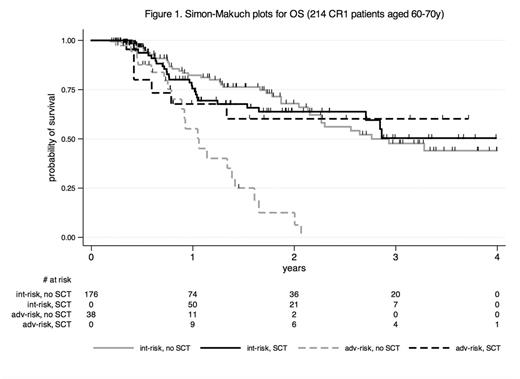
Role of SCT - Among the 305 CR patients eligible for SCT, 93 proceeded to SCT in CR1. In addition, 22 patients with primary refractory AML and 25 patients relapsing prior to SCT eventually received SCT. Patients transplanted in CR1 were younger (median age, 64 [60-73] vs 70 [60-81] years; p<0.001) and had lower comorbidity index (HCT-CI≥3, 14 vs 26%; p=0.025) than the remaining eligible patients. We thus analyzed the role of SCT in CR1 in the 214 eligible patients aged 70 years old or less (ELN-risk: 2 favorable, 176 intermediate, 38 adverse). Ninety of them were actually transplanted in CR1 (ELN risk: 75 intermediate, 15 adverse; median time from CR to SCT, 113 days; stem cell source: 28 geno-id, 50 pheno-id, 8 haplo-id, 4 cord blood; conditioning regimen: 12 NMA, 66 RIC, 12 sequential-RIC). These 90 transplanted patients were still younger than the 124 non-transplanted patients (p=0.005) but their ELN-risk and HCT-CI distribution were similar. Among them, 22 patients relapsed and 29 died, including 18 deaths in CR1. At 2 years post-SCT, transplant related mortality (TRM) was 20.4% (95% CI, 13.2-30.9), cumulative incidence of relapse was 22.7% (95% CI, 15.0-33.4), and OS was 65.1% (95% CI, 52.9-75.0). Age, secondary AML, ELN-risk, type of stem cell source, or conditioning regimen did not significantly influence post-transplant survival. In a time-dependent SCT analysis, OS was not significantly prolonged in the SCT cohort (HR, 0.77 [95% CI, 0.49-1.21]; p=0.26). As illustrated on Figure 1, an OS benefit associated with SCT was only observed in the adverse ELN-risk subset (HR, 0.20 [95% CI, 0.07-0.63]: p=0.006), while not in the intermediate ELN-risk subset (HR, 1.08 [95% CI, 0.65-1.80]; p=0.76), with a significant interaction (p=0.005). Finally, SCT did not significantly prolonged OS in the 47 out of 319 patients with refractory/relapsed AML who eventually received SCT (HR, 0.69 [95% CI, 0.39-1.22]: p=0.21).
Conclusion - In older AML patients, due to persistent high TRM and relapse incidence, RIC-SCT significantly prolongs survival in the adverse ELN-risk AML subset only. Even if a longer follow-up is needed, patients with intermediate ELN-risk AML do no seem to benefit from SCT in CR1 as compared to standard chemotherapy.
De Botton: Servier: Honoraria; Pfizer: Honoraria; Novartis: Honoraria; Celgene: Honoraria; Agios: Honoraria, Research Funding. Socié: Alexion Pharmaceuticals, Inc.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal